Background:
Extracorporeal membrane oxygenation (ECMO) is a salvage therapy for critically ill children and adults. Hematologic complications, such as hemorrhage and thrombosis, are the major complications in ECMO. The contact of blood with the tubing of the circuit, lines, blood pump, and oxygenator all contribute to the process. Most patients require anticoagulation while on ECMO. According to the international summary of Extracorporeal Life Support Organization (ELSO) registry in 2017, patients on ECMO consist of 69% neonate and pediatric patients (Neo 44.8%, Peds 24.1%, Adult 31.1%).
Contributors to the risk of bleeding include excessive heparin use for systemic anticoagulation, consumption of coagulation factors, low fibrinogen levels, thrombocytopenia, platelet dysfunction, and hyperfibrinolysis, among others. This gives the appearance of a consumptive coagulopathy, the hallmark of which is hypofibrinogenemia. Fibrinogen replacement is most efficiently done with cryoprecipitate (cryo) or fibrinogen concentrate, while fresh frozen plasma (FFP) has a low and variable fibrinogen content. Cryo and FFP may contribute to volume expansion and have other prothrombotic factors which could contribute to thrombotic complications.
We performed a retrospective analysis of pediatric and adult patients who presented for ECMO to evaluate management of low fibrinogen and bleeding and thrombotic complications.
Methods:
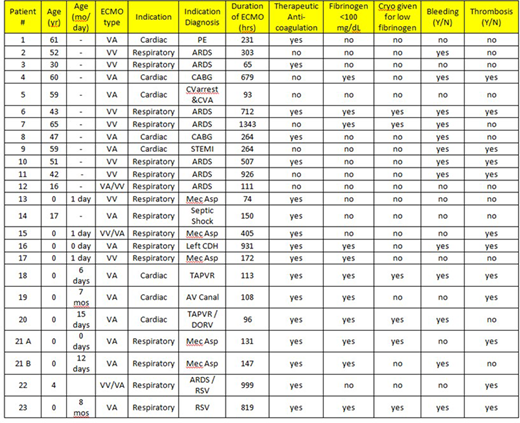
Data was reviewed for 11 adult and 12 pediatric consecutive patients who received ECMO prior to June 1st, 2019. Time on ECMO (hours), type of ECMO, indication, presence of bleeding or thrombotic complications during ECMO, and use of therapeutic anticoagulation was collected. Laboratory data included platelet counts, hemoglobin, fibrinogen activity, antithrombin activity, prothrombin time, and partial thromboplastin time. Transfusion data was also collected for amount of packed red blood cells (PRBC), platelets, FFP, and cryo transfused.
Data were analyzed to evaluate when fibrinogen was low and if cryo was given. According to our institutional guideline, the fibrinogen activity goal is >100 mg/dL and >200 mg/dL if bleeding. Bleeding and/or clotting complications were also noted.
Data:
There were 24 runs of ECMO evaluated (11 adults, 12 children), including VA and VV, lasting from 65-1343 hours. One child had 2 runs of ECMO. The majority were VA (13/24; 54%) with 33% (8/24) VV and 13% (3/24) combined VA/VV (all occurred in children). Therapeutic anticoagulation was given in 17/24 (71%) overall, but 92% (12/13) of pediatric cases. Bleeding and/or clotting complicated 17 (71%) runs. Overall, bleeding occurred in 13 (54%) runs and thrombosis in 12 (50%). Of these events, 8 (33%) runs had both bleeding and thrombosis. Bleeding occurred in 8/11 (73%) adults and 5/12 (42%) children. Bleeding and/or thrombus occurred more often with longer ECMO runs, but affected all runs longer than 250 hours (12/24, 50%).
While on ECMO, the fibrinogen activity was below 100 mg/dL at some point in 11/24 (46%) of runs. Of those 11, only 6 (55%) received cryo in response to the fibrinogen activity. Cryo was more likely to be given if both a low fibrinogen and bleeding were present. Even with bleeding episodes and fibrinogen activities <200 mg/dL, cryo was not given in the majority of cases (70% adults, 40% children), but FFP was given preferentially.
Conclusions:
Almost half (45%) of the patients evaluated had low fibrinogen levels at some point while on ECMO. Despite cryoprecipitate being standard replacement at our institution for low fibrinogen, only 55% of those patients received cryo in response to the low level. Therefore, 21% (5/24) of all cases were not specifically treated for their low fibrinogen value. Bleeding and/or thrombotic complications are common with ECMO. Further study to determine if fibrinogen replacement or lack thereof contributes to these complications and guide management of fibrinogen deficiency in ECMO patients is warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.